Perforated Ogilvie’ syndrome. A rare paraneoplastic manifestation of small cell lung cancer secreting ACTH
WCRJ 2014; 1 (2) : e206
Topic: Surgical oncology
Category: Case report
Abstract
CASE DESCRIPTION: A 59 years old woman, with a six months history of hypercortisolism, has been diagnosed with Small Cell Lung Carcinoma (SCLC) secreting ACTH. After the first cycle of chemotherapy the patient showed an acute intestinal obstructive syndrome. The CT scan showed an exceedingly dilated colon (cecum 13.9 cm and transverse colon 10 cm). The physical and laboratory findings led to laparotomy and perforations of both the cecum and the transverse colon were found. A subtotal colectomy with ileocolic anastomosis was performed. The patient was discharged on postoperative day 15. After a second cycle of chemotherapy she had further worsening and died 55 days after surgery.
DISCUSSION: Small Cell Lung Carcinoma is frequently associated with paraneoplastic syndromes, related to ectopic endocrine activity or to immunologic changes. Autoimmune impairment and destruction of the myenteric plexus by antineuronal, anti-Calcium-Channel, anti Cajal-cell antibodies have been described in patients with SCLC. These alterations are usually the cause of gastrointestinal dysmotility in lung cancer patients. The electrolytic imbalance, typical of the endocrine syndromes, is also a known pathogenetic factor of Ogilvie’ syndrome.
Obstruction can respond to medical treatment or to colonoscopic decompression but recurrence are frequent and ischemia and perforation can develop. The prognosis is overall poor and in the presence of endocrine disfunctions, dismal. After perforation mortality rate further rises.
Abbreviations: ACPO, Acute Colonic Pseudo-Obstruction; OS, Ogilvie’ syndrome; SCLC, Small cell lung cancer; POMC, Proopiomelanocortin.
BACKGROUND
Acute colonic pseudo-obstruction (or ACPO, Ogilvie’ syndrome) is a clinical syndrome well known but still not well understood, whose specific pattern is the acute dilation of the colon without mechanical obstructions.
Usually we distinguish a primary syndrome and a secondary one. The first one includes myopathies and neuropathies. The second group can be caused by various metabolic, degenerative, endocrine, pharmacological or iatrogenic causes.
In the case here reported, the pseudo-obstruction complicated by perforation is the ultimate manifestation of an endocrine paraneoplastic syndrome due to a small cell lung carcinoma (SCLC) secreting ACTH.
THE CASE
A 59 years old woman was admitted to our unit in October 2006 for abdominal pain and distension three days history of constipation, nausea and vomiting.
The patient had a prolonged history of tobacco abuse, post-surgical hypothyroidism on substitutive therapy with L-Thyroxin. During the last six months she reported a significant weight loss (7 kg), nausea, vomiting and she was diagnosed with new onset hypertension. Esophagogastroduodenoscopy and colonoscopy were negative. Laboratory analysis showed hyponatremia (Na 126 mmol/L), Hypokalemia (3 mmol/L), Hypercortisolemia (436 ng/ml) leading to further endocrinologic studies, including dexamethasone suppression test and circadian rhythm of Cortisol. The studies confirmed hypercortisolemia without increased ACTH levels (18.6 pg/ml). A CT demonstrated a large left lung mass with left adrenal lesion and the bronchoscopic biopsy confirmed the suspected Small Cell Lung Carcinoma (SCLC). The hypercortisolemia was considered to be paraneoplastic, but it was impossible to confirm ACTH hypersecretion. Thus she was discharged home with Ketoconazole, (to reduce secretion of adrenal cortical hormones), KCl 60 mEq/die, domperidone and ondansetron. A careful review of her charts showed a previous episode of intestinal obstruction. She then underwent to her first cycle of chemotherapy. Soon after she presented with symptoms of intestinal obstruction, for which she was admitted to our Surgical Unit.
At admission, her physical examination showed signs of significant weight loss, dehydration, and a conspicuous abdominal distension with visible intestinal loops, marked abdominal tenderness and no bowel sounds.
A non operative approach with fluid resuscitation and nasogastric decompression was initially taken. After an initial bladder residual of 600 ml, the patient had normal diuresis.
The laboratory analysis showed a RBC count of 3,540,000, WBC 4,890, HGB 9.7, PLT 547,000, Na 130 mmol/L, K 3.41 mmol/L, Cl 92 mmol /L.
The radiological examination of the abdomen showed large air-fluid levels in the upper quadrants and a massive colonic distension, while the chest x-ray showed a mass of the left hilum with multiple parahilar opacities. The repeat CT scan of the chest abdomen and pelvis showed an irregular mass of 10 cm in longitudinal diameter with heterogeneous contrast enhancement in the left lung. The right and transverse colon were dilated (respectively 13.9 cm and 10 cm) with an incompetent ileocecal valve, as shown by multiple dilated loops of small bowel (Figure 1 A and B). Several lesions suspicious for metastasis were seen in the head of pancreas; also the adrenal lesion was considered to be metastatic in origin. The liver, instead, was free from secondary lesions.
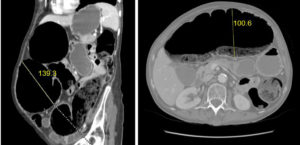
Figure 1. CT scan: CT scan showed the right (A) and transverse colon (B) dilated (respectively 13 cm and 10 cm) with an incompetent ileocecal valve, as shown by multiple dilated loops of small bowel.
In spite of the absence of free air, or free fluid on CT scan, the clinical findings of acute abdomen with significant dilatation of the cecum, the ascending and transverse colon, posed the indication for laparotomy. The intraoperative findings were noticeable for purulent fluid in the peritoneal cavity, due to a partially contained perforation of the cecum and of the proximal transverse colon. A subtotal colectomy was then performed with stapled ileocolic anastomosis.
After three days in the intensive care unit, the patient returned to the ward, without any complications.
The patient’s renal function remained normal, however a continuous electrolyte replacement of was necessary to keep serum electrolytes at normal values.
The bowel function returned on the fifth postoperative day. The patient was discharged on the fifteenth postoperative day.
The pathology was consistent with diffuse mucosal ulcerations and multiple perforations of cecum and transverse colon, degeneration of the myenteric plexus secondary to the massive inflammation and hypotrophy of the muscular layer, typical of Ogilvie’ syndrome.
A week after discharge, the patient underwent to the second cycle of Chemotherapy. Then she presented with a worsening of her hydroelectrolictic imbalance, lethargy and progressive multiorgan failure and eventually died 55 days later.
DISCUSSION
Among all cancers, small Cell Lung Carcinoma (SCLC) is the neoplasia most frequently associated with paraneoplastic syndromes.
These syndromes can be caused by ectopic secretion of endocrine substances (especially ACTH-like molecules) or by an immunological cross-reactivity to neoplastic cells antigens. The latter cases have, usually, a better prognosis than the former.
In the case here described the patient presented with almost all the possible paraneoplastic syndromes, and ultimately, she developed an acute intestinal pseudo obstruction or Ogilvie’ syndrome complicated by perforation.
The initial presentation of her disease was with gastrointestinal symptoms, such as anorexia, nausea, vomiting and weight loss. All the above mentioned symptoms have been well correlated with paraneoplastic gastrointestinal dysmotility. Some cases have been reported of autoimmune impairment and destruction of the myenteric plexus by antineuronal, anti-Calcium-Channel, anti Cajal-cell antibodies in patients with SCLC 1 , 2. In some other case the impairment was due to inflammatory infiltration by B-cell and T-cell lymphocytes without gross neuronal abnormalities 3.
Her weight loss, together with polyuria and hypertension, is also expression of acute hypercortisolism, as confirmed by the negative response to dexamethasone suppression test. The cause of this hypercortisolism in lung cancer is usually due to ectopic secretion of ACTH that reaches higher values than in pituitary syndromes 4. In spite of the elevated ectopic production of ACTH, it can be difficult to demonstrate the increase, unless an immunostaining of the neoplastic tissue is performed 5. The ectopic ACTH syndrome is characterized by overexpression and aberrant posttranslational processing of proopiomelanocortin (POMC), with release of ACTH precursors, but not always ACTH itself. The gross elevation of precursors is sufficient to induce hypercortisolemia 6.
Although our patient had an adrenal metastasis, there is no proof that this was responsible for the hypercortisolism. In general, patients with adrenal metastasis from lung cancer present with subclinical Cushing’ syndrome, at most 7, and only a very small percentage of these patients are symptomatic (4% according to the study of Lam et al) 8. Furthermore, none of the metastatic lesions to the adrenals are hyperfunctional 9.
The severe hypokalemia is also a consequence of her hypercortisolism, and the imbalance in itself can be the only cause of acute pseudo-obstruction.
Pseudo-obstruction itself (chronic or acute) has been already reported as part of paraneoplastic syndrome in SCLC with immunological pathogenesis 10 , 11 , 12.
Spontaneous perforation is the most feared complication of the syndrome, and occurs in 3-15% of patients with a mortality rate of 40-50% 13. Although a dilated cecum over 12 cm and a transverse colon more than 8-9 cm have been described to be at high risk for perforation 14, the colonic diameter alone should not be considered a predictive factor. In fact, some authors describe cancer patients with ACPO with larger cecal diameters (9-18 cm) without perforation or need for endoscopic or surgical decompression 15.
More reliable parameters are the duration of the symptoms (more than 6 days) and the presence of marked tenderness at physical examination. Also the persistence or progression of symptoms after rehydratation, administration of neostigmine or failure of endoscopic decompression can require a surgical decompression 16.
Although it is true that the presence of free air or free fluid in the abdomen is indicative of a perforation, their absence does not completely rule that out. Also radiologic investigation, such us erect X-rays and CT scan can fail to show the free air of recent or sealed perforations 17 , 18. Indirect signs of perforation can be found on CT scan in the form of inflammatory changes in the pericolonic soft tissues.
When necessary, many different surgical options have been proposed, such as laparoscopic decompression with cecostomy, limited colonic resection and subtotal or total colectomy with ileorectal anastomosis. The nature and the extent of the lesion will determine the type of resection 19.
The often extreme severity of the underlying illness forces the surgeon to choose the least invasive technique. In some patient the best option is the resection, since often Ogilvie’ syndrome has a tendency to recur and perforate 20.
The acute colonic pseudo-obstruction resulting from endocrine imbalance can fail to respond to therapy and, when the underlying cause is lung cancer, the prognosis remain dismal.
Competing interests
The authors declare that they have no competing interests.
Consent
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Pardi DS, Miller SM, Miller DL, Burgart LJ, Szurszewski JH, Lennon VA, Farrugia G. Paraneoplastic dysmotility: loss of interstitial cells of Cajal. Am J Gastroenterol 2002; 97: 1828-1833. (back)
- Lee HR, Lennon VA, Camilleri M, Prather CM. Paraneoplastic gastrointestinal motor dysfunction: clinical and laboratory characteristics. Am J Gastroenterol 2001; 96: 373-379. (back)
- Jun S, Dimyan M, Jones KD, Ladabaum U. Obstipation as a paraneoplastic presentation of small cell lung cancer: case report and literature review. Neurogastroenterol Motil 2005; 17: 16-22. (back)
- Blunt SB, Sandler LM, Burrin JM, Joplin GF. An evaluation of the distinction of ectopic and pituitary ACTH dependent Cushing’s syndrome by clinical features, biochemical tests and radiological findings. Q J Med 1990; 77: 1113-1133. (back)
- Mussig K, Hoger M, Haring HU, Wehrmann M. Syndrome of inappropriate antidiuretic hormone secretion and ectopic ACTH production in small cell lung carcinoma. Lung Cancer 2007; 57: 120-122. (back)
- Wajchenberg BL, Mendonça B, Liberman B, Adelaide M, Pereira A, Kirschner MA. Ectopic ACTH syndrome. J Steroid Biochem Mol Biol 1995; 53: 139-151. (back)
- Tsvetov G, Shimon I, Benbassat C. Adrenal incidentaloma: clinical characteristics and comparison between patients with and without extradrenal malignancy. J Endocrinol Invest 2007; 30: 647-652. (back)
- Lam KY, Lot CY. Metastatic tumors of adrenal glands: a 30-years experience in a teaching hospital. Clin Endocrinol 2002; 56: 95-101. (back)
- Lam KY, Lot CY. Metastatic tumors of adrenal glands: a 30-years experience in a teaching hospital. Clin Endocrinol 2002; 56: 95-101. (back)
- Chu G, Wilson PC, Carter CD, Lennon VA, Roberts-Thomson IC. Intestinal pseudo-obstruction, type 1 anti-neuronal nuclear antibodies and small-cell carcinoma of the lung. J Gastroenterol Hepatol 1993; 8: 604-606. (back)
- Oneschuk D. Colonic pseudo-obstruction in a patient with advanced small cell carcinoma. J Palliat Care 2002; 18: 202-204. (back)
- Simpson DA, Pawlak AM, Tegmeyer L, Doig C, Cox D. Paraneoplastic intestinal pseudo-obstruction, mononeuritis multiplex, and sensory neuropathy/neuronopathy. J Am Osteopath Assoc 1996; 96: 125-128. (back)
- Saunders MD. Acute colonic pseudo-obstruction. Best Pract Res Clin Gastroenterol 2007; 21: 671-687. (back)
- Coulie B, Camilleri M. Intestinal pseudo-obstruction. Annu Rev Med 1999; 50: 37-55. (back)
- Sloyer AF, Panella VS, Demas BE, Shike M, Lightdale CJ, Winawer SJ, Kurtz RC. Ogilvie’s syndrome. Successful management without colonoscopy. Dig Dis Sci 1988; 33: 1391-1396. (back)
- Jain A, Vargas HD. Advances and challenges in the management of acute colonic pseudo-obstruction (Ogilvie syndrome). Clin Colon Rectal Surg 2012; 25: 37-45. (back)
- Kim HC, Shin HC, Park SJ, Park SI, Kim HH, Bae WK, Kim IY, Jeong D S. Traumatic bowel perforation. Clin Imaging 2004; 28: 334-339. (back)
- Yeung KW, Chang MS, Hsiao CP, Huang JF. CT evaluation of gastrointestinal tract perforation. Clin Imaging 2004; 28: 329-333. (back)
- Jain A, Vargas HD. Advances and challenges in the management of acute colonic pseudo-obstruction (Ogilvie syndrome). Clin Colon Rectal Surg 2012; 25: 37-45. (back)
- Catena F, Caira A, Ansaloni L, Calò G, De Bonis F, Agrusti S, D’Alessandro L, Taffurelli M. Ogilvie’s Syndrome treatment Acta Bio Medica 2003; 74(Suppl. 2): 26-29. (back)
To cite this article
Perforated Ogilvie’ syndrome. A rare paraneoplastic manifestation of small cell lung cancer secreting ACTH
WCRJ 2014; 1 (2) : e206
Publication History
Published online: 30 Jun 2014

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.